Key Points:
Symptoms of both conditions can vary from person to person, and flare-ups may come and go.
- Early medical care can help slow progression in rheumatoid arthritis and prevent severe disability.
- There is no cure for osteoarthritis or rheumatoid arthritis, but early and ongoing treatment can significantly improve quality of life.
- Ongoing research and clinical trials continue to explore new and safer treatment options for both conditions.
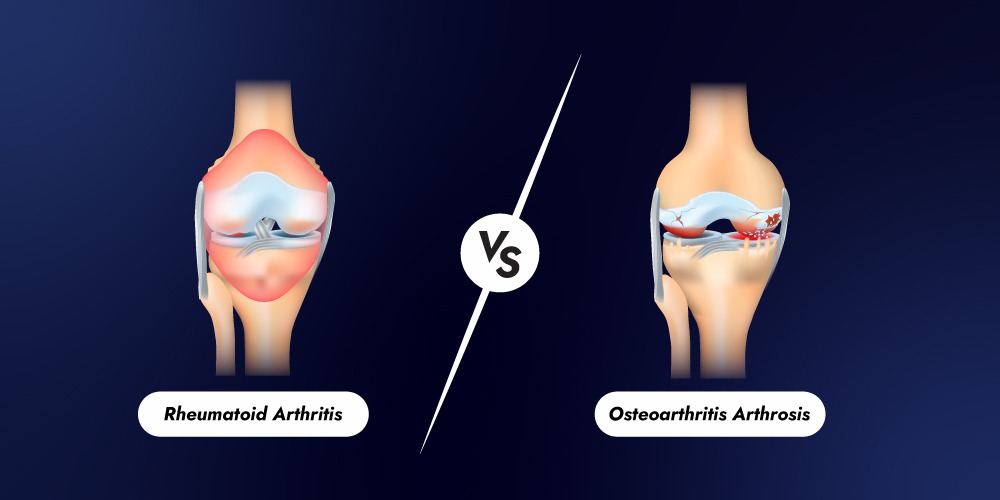
Difference Between Osteoarthritis and Rheumatoid Arthritis
Although both conditions cause joint pain and stiffness, osteoarthritis and rheumatoid arthritis develop for entirely different reasons.
Osteoarthritis: A Degenerative Joint Condition
Osteoarthritis is often described as a “wear and tear” disease. It develops when the protective cartilage that cushions the bones gradually breaks down. As the cartilage wears away, the bones begin to rub against each other, causing pain, stiffness, and reduced movement. Risk factors for osteoarthritis include aging, excess body weight, joint injuries, repetitive joint use, and family history. Because OA is not caused by immune system dysfunction, it usually does not involve widespread inflammation throughout the body. This usually affect the bones that bear weight or are used repeatedly, such as:
- Knees
- Hips
- Lower Back
- Hands
Symptoms tend to worsen slowly over time and are often linked to ageing, obesity, prior to joint injury, or repetitive stress on the joints.
Rheumatoid Arthritis: An Immune Disease
Rheumatoid arthritis, on the other hand, is an autoimmune disorder. Instead of protecting the body, the immune system mistakenly attacks the lining of the joints. This leads to inflammation that can damage cartilage, bone, and surrounding tissues. it can also affect organs like the lungs, heart, and eyes, making it a systemic disease.
Unlike osteoarthritis, RA often causes prolonged morning stiffness, lasting more than 30 minutes. Many people also experience fatigue, weakness, and general discomfort even before joint symptoms become severe.
RA can appear suddenly or develop gradually and may affect people in their 20s, 30s, or 40s.
Key Differences at a Glance
| Feature | Osteoarthritis | Rheumatoid Arthritis |
|---|---|---|
| Cause | Cartilage breakdown | Immune system attack |
| Progression | Gradual | Can be rapid |
| Age of onset | Usually older adults | Any age |
| Joint pattern | Often one side | Usually symmetrical |
| Morning stiffness | Short-lived | Lasts longer than 30 minutes |
| Whole-body symptoms | Rare | Common (fatigue, fever) |
Seronegative Rheumatoid Arthritis & Seropositive Rheumatoid Arthritis
Doctors often use blood tests to help diagnose rheumatoid arthritis. These tests look for specific antibodies, including rheumatoid factor (RF) and anti-CCP antibodies. However, not everyone with RA tests positive for these markers.
When a person shows clear symptoms of rheumatoid arthritis but does not have detectable antibodies, the condition is called seronegative rheumatoid arthritis. This does not mean the disease is imaginary or less serious. Many seronegative patients experience joint inflammation, pain, and functional limitations similar to those with seropositive RA.
Over time, some individuals initially diagnosed as seronegative may later develop detectable antibodies. Treatment for seronegative RA typically follows the same approach as seropositive RA, focusing on reducing inflammation and slowing disease progression.
Seropositive rheumatoid arthritis occurs when blood tests detect RF, anti-CCP antibodies, or both. This form of RA is more common and often associated with a higher level of immune activity.
Patients with seropositive RA may be at greater risk for joint damage and complications outside the joints, such as rheumatoid nodules or cardiovascular involvement. The presence of antibodies helps confirm the diagnosis and may guide treatment decisions, especially when selecting disease-modifying medications.
Rheumatoid Arthritis Clinical Trials
Access Research-Based Treatment Options for Rheumatoid Arthritis
Clinical trials may provide access to investigational therapies aimed at reducing inflammation and improving joint function.
Risk Factors for Osteoarthritis and Rheumatoid Arthritis
Although osteoarthritis and rheumatoid arthritis both affect the joints; their risk factors are different because the causes are different.
Risk Factors for Osteoarthritis
Osteoarthritis develops gradually due to stress on the joints over time. Common risk factors include:
- Age: Risk increases as you get older
- Joint overuse: Repetitive movements from work or sports
- Previous joint injury: Fractures or ligament injuries
- Excess body weight: Extra weight puts more pressure on joints, especially knees and hips
- Family history: Genetics can play a role
Risk Factors for Rheumatoid Arthritis
Rheumatoid arthritis is linked to immune system dysfunction. Known risk factors include:
- Gender: More common in women
- Genetics: Certain genes increase risk
- Smoking: Strongly associated with RA development
- Hormonal factors: Pregnancy or menopause may influence risk
- Autoimmune tendency: Personal or family history of autoimmune diseases
Treatment for Osteoarthritis & Rheumatoid Arthritis
There is currently no cure for either osteoarthritis or rheumatoid arthritis, and existing joint damage cannot be reversed. Treatment for both conditions focuses on relieving pain, reducing stiffness, and improving joint function. In rheumatoid arthritis, the main goal of treatment is to slow disease progression and control the immune system, which mistakenly attacks the joints. In osteoarthritis, treatment aims to reduce stress on the joints and manage symptoms. Common treatment approaches for both conditions include pain-relieving medications, the use of heat or ice to ease discomfort, and regular, low-impact exercise. For people with osteoarthritis, weight loss may also be recommended to reduce pressure on affected joints and improve mobility.
Rheumatoid Arthritis Clinical Trials
Rheumatology clinical trials focus specifically on understanding and treating RA. Rheumatoid Arthritis clinical trials help researchers understand disease mechanisms and evaluate new treatments, diagnostic tools, and management strategies. These may involve early-phase safety studies or large-scale trials comparing new treatments with standard care. Participants often receive close medical monitoring and contribute valuable data that can shape future treatment guidelines. Hospitals and research institutions across the state conduct numerous clinical trials in Massachusetts, including studies focused on rheumatoid arthritis and other autoimmune diseases. By participating in clinical research, individuals help improve understanding of arthritis and contribute to the development of better treatments for future patients.
Rheumatoid Arthritis Clinical Trials
Access Research-Based Treatment Options for Rheumatoid Arthritis
Clinical trials may provide access to investigational therapies aimed at reducing inflammation and improving joint function.
Ongoing Arthritis Studies at Lucida Clinical Research
Lucida Clinical Research actively supports and conducts clinical trials aimed at improving care for people with rheumatologic conditions, including rheumatoid arthritis. Through carefully designed studies and patient-centered research practices, Lucida Clinical Research contributes to the development of potential treatment options.
We follow strict clinical trials safety regulations to protect participants. These regulations ensure that studies are ethical, transparent, and scientifically sound. Participation in these studies not only provides access to advanced medical care but also helps expand scientific knowledge that benefits the wider arthritis community.
Final Thoughts
While osteoarthritis and rheumatoid arthritis may share similar symptoms, they are fundamentally different in conditions. Osteoarthritis results from joint degeneration over time, while rheumatoid arthritis is an autoimmune disease driven by chronic inflammation. Understanding these differences is essential for early diagnosis, appropriate treatment, and informed healthcare decisions.
Ongoing clinical research continues to improve outcomes for people living with arthritis. Whether through education, treatment, or participation in clinical trials, knowledge remains a powerful tool in managing joint health.